If you and your partner have been trying to get pregnant and it’s just not happening—it’s okay. You’re not alone.
About 1 in 7 couples worldwide face infertility, and contrary to common belief, it’s not just a women’s issue. In fact, in many cases, the reason can be male factor infertility. That’s why understanding and addressing male infertility is just as important—and yes, also very treatable.

Male infertility simply means a man’s sperm isn’t able to fertilize the egg. This could be due to low sperm count, poor sperm quality, or blockages that stop sperm from reaching the egg. In India, lifestyle factors like smoking, alcohol, pollution, stress, and obesity can all contribute to it. Health conditions like diabetes and untreated infections can also be the reason why.
Sometimes sperm is produced—but can’t get out. This can happen due to previous surgeries, infections, or congenital issues.
Smoking, alcohol, drugs, obesity, heat exposure, and stress—can all reduce fertility levels.
Your healthcare provider will find out about your health, lifestyle, past infections or injuries, and sexual function.
Checking the testicles and penis for any abnormalities like varicocele or signs of hormonal imbalances.
A simple test to evaluate your sperm count, movement, shape, and semen volume. This may be done more than once to get accurate results.
To check hormone levels like testosterone, FSH, LH, and thyroid hormones.
To look for blockages, tumors, or varicoceles.
If your sperm count is very low or zero, you may be asked to get tested for Y chromosome issues or conditions like Klinefelter’s.
To check if semen is going into the bladder (retrograde ejaculation).
In some cases, a small tissue sample is taken to check if sperm is being produced.
To look at DNA damage or the sperm’s ability to fertilize an egg.
Infertility doesn’t always need complex treatments. Sometimes, small lifestyle changes go a long way:
If you’re struggling with infertility, don’t wait. Early diagnosis makes a big difference.
PCOS is a hormonal and Metabolic condition that affects women […]
04 Jun 22

IUI is a simple form of fertility treatment where motile […]
06 Aug 22
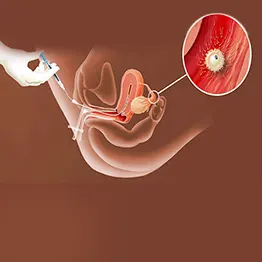
We are happy to have treated more than 20,000 couples with fertility issues. IUI is simple treatment for couples with unexplained Infertility, PCOS, early endometriosis Know More
Indicated in couples with tubal blockage, repeated failed IUI and endometriosis. Results range across 40 -50% at our centre Know More
Treatment of choice for male infertility with very low sperm count, obstructive azoospermia and for coupes requiring donor eggs. Know More
Many young men and women have utilized our fertility preservation services in the form of sperm, egg and embryo freezing either for medical or social reasons Know More

More than 3000 women have delivered at our centre. They have had an exceptional experience in antenatal care, delivery and postnatal care. Know More
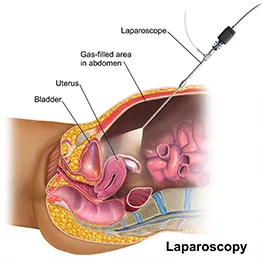
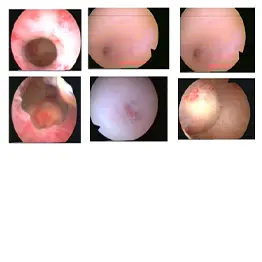
We have been performing all Gynaec surgeries through Laparoscopy for the past 25 years. Advantages are it is safe, less painful Know More
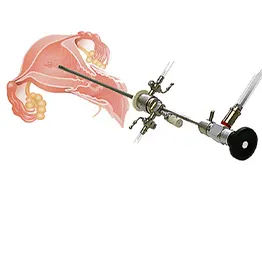
Hysteroscopy has many advantages over traditional D & C. We are equipped with small telescope to diagnose and treat pathologies inside the uterine cavity Know More
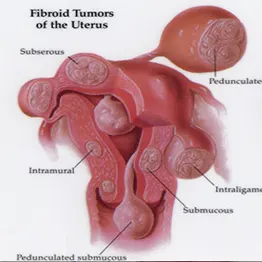
Fibroid causes infertility, pain and excessive menstrual blood loss. They can be operated through Laparoscopy or Hysteroscopy Know More
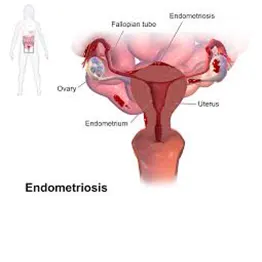
Endometriosis causes infertility and painful periods. Best treatment is initiated by Laparoscopy surgery and drugs Know More

We have been performing laparoscopic hysterectomy for the past 25 years. It is a definitive treatment for heavy menstrual bleeding, fibroids, cancer Know More
Ectopic is a condition where the pregnancy gets implanted in the fallopian tube instead of the uterine cavity. We have operated many cases laparoscopically Know More
Hysteroscopy helps in evaluating the cause of Postmenopausal bleeding Know More

MD. DGO.,
Gynaec Endoscopy Surgeon Fertility and IVF Consultant

M.S. Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound

MS, DNB Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound
-Very satisfied.
-Doc Support indeed was very good .
-Nurse Support was absolutely Beneficial and excellent.
-Cleanliness was upto the mark.
-Hospitality made the stay comfortable.
KEEP IT UP!
Harshita Chhajed
We were so ecstatic on 9thapril 2022 as we hold our baby boy in our hands. We are so grateful as we were in the bestest and safest hands. All this was possible because of the talented doctors like you all-Dr Sudha Tandon, Dr Aditi Tandon, Dr Amrita Tandon and Dr Sachin. Dr Sudha Tandon and DrAditi Tandon helped us in our pregnancy journey by making themselves available all the time on phone. All our queries/questions were answered in no time which is by far the best response we could have received during covid times.
All doctors have given us bestest suggestions during our pregnancy journey in which we always had an utmost faith. It was a great time spent with you all during this pregnancy.
Thankyou so much for all the help/assistance/suggestions. We will always recommend Dr Tandon to our friends and relatives.
Sheela C Potdar
Dr Sudha Tandon and her two daughters make you feel comfortable and at ease. The flow of the process was smooth without making the patients wait unnecessarily.
Ashrita Katyal
Staff very polite and cordial.
Clean and neat hospital.
Cheerful ambience.
Doctor was very cooperative understanding and most importantaly non-judgemental. Made talking easier.
Thankyou for this wonderful offer and for making these tests accessible to all.
Odette Fred
-Staff very pleasant and polite.
-Dr too very polite.
-No waste of time.
-Clean place.
-Gives a good feel and not a nervous hospital feel.
Rosa Fred
Dr Sudha Tandon is one of the most oldest and the bestgynac in Chembur. Very good initative taken by them to keep a watch on the womenshealth on the occasion of the womensday.glad to see her daughters doing the job same as their mom.
All the best to both of them.
Thankyou
Satpal Bhambri
Thankyou for arranging this camp and providing services at affordable prices. The entire doctors team and also everyone right from the front desk staff to the staff nurses are really very cordial and soft-spoken.
My mother literally has a OBGY phobia :-o yet when she stepped out of the consulting room,she only told me they are all really great especially Dr AditiMaam.
Keep up the good work! I always recommend your name whenever any relatives/friends ask for a good OBGY in town.
Thankyou
Regards,
Dr Aditi Prabhu
Pratima Prabhu
-Very well organized.
-The staff is very competent.
-Quick process without any difficulties.
-Excellent time Management.
Kavita Bhatti
It is always reassuring to talk to Dr Sudha Tandon, Dr Amrita and Dr Aditi. It is for their expert advise and their compassionate approach that makes me come back to them for all my health related concives. I know I am in good hands.
Sheetal Patil
Thank you for this camp. Was done professionally and good staff.
Thanks again.
Kavita R.
Got to hear from a friend about this women’s day camp. Very well organized camp by Dr Sudha Tandon.
The price works well for all.
Thank-you
Mrs. Harvinder Saggi
I was absolutely satisfied with Doctor Amrita’s Consultation.
She cleared all my queries.
Thank you for having this women’s day camp.
Its really helpful.
Gunwant Saggi
My mother has also been Dr Sudha Aunty’s patient and it was but natural for me to follow same.I would like too extend my gratitude and thanks to Dr Sudha aunty for being there for me at every step.My sincere thanks to Dr Aditi and Dr Amrita who have always had my back and responded to every query and doubt with great promptness. Dr Aditi has been my “go-to-person” in times of anxiety.
A big thank you to all three of there for everything. I couldn’t have pulled this off without your support.
Dr Jayeeta Verma