Uterine fibroids are a common kind of growth that can grow in and on your uterus. They are not cancerous. These are growths made of muscle and tissue that form in or on the wall of your uterus. They are also known as leiomyomas. These growths are most often benign (not dangerous) and are the most common benign tumor in women.
Uterine fibroids can cause a lot of different signs, such as pain and heavy, irregular bleeding in the uterus. People with fibroids don't always know they have them because they don't have any signs. How you are treated for fibroids usually depends on how bad your symptoms are.
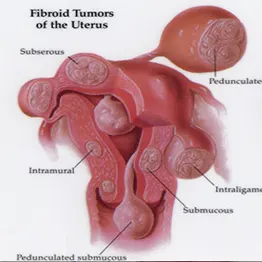
Types of Uterine FibroidsUterine fibroids are classified into several categories based on their location and attachment method. There are several forms of uterine fibroids, including:
A lot of people who have uterine fibroids don't even know they have them. The signs and symptoms can be changed by where, how big, and how many fibroids a person has.
These are the most frequent signs of uterine fibroids:
Often, fibroids are put into groups based on where they are. Inside the muscle wall of the uterus, intramural fibroids grow. Fibroids under the mucosa push into the uterine region. Those that are subserosal form on the outside of the uterus.
It's not clear what causes uterine tumours. But these things may play a part:
Medics think that uterine fibroids might start in a stem cell in the uterus's smooth muscle tissue. Cells split over and over again. Over time, it changes into a firm, rubbery mass that is different from the flesh around it.
Uterine tumours grow in a number of different ways. They could grow quickly or slowly. They could also stay the same size. Some fibroids get bigger, and some get smaller on their own.
When a woman gives birth, her uterus shrinks and is back to its normal size. This can cause fibroids to shrink or go away.
There are various risk factors that can influence your chances of acquiring fibroids. These may include:
In many situations, a healthcare provider detects uterine fibroids during a pelvic exam. Quite often, excessive bleeding and other related symptoms may prompt your provider to consider fibroids as a component of the diagnosis. Fibroids can be confirmed and their size and location determined by tests. Tests may include:
Treatment for uterine fibroids varies according to their size, quantity, and location, as well as the symptoms they cause. If you don't have any symptoms from your fibroids, you may not require treatment. Small fibroids can frequently be left alone. Some people have no symptoms or issues related to fibroids. In these circumstances, your doctor may advise you to get regular pelvic exams or ultrasounds to monitor your fibroids.
If you have fibroids-related symptoms, such as anemia from excessive bleeding, moderate to severe discomfort, or urinary tract and bowel difficulties, you will need to seek treatment. Your treatment strategy will be determined by several factors, including:
The most appropriate treatment option for you will also be determined by your future pregnancy goals. When discussing treatment choices with your doctor, talk about your fertility goals. Treatment options for uterine fibroids may include:
Any drug you take should be discussed with your healthcare professional. Always with your doctor before beginning a new medicine to discuss any potential concerns.
When comparing the various methods of fibroid removal surgery, several aspects must be considered. Not only can the size, location, and number of fibroids influence the type of surgery, but your future pregnancy goals should also be considered when formulating a treatment strategy. Some surgical options keep your uterus intact and allow you to conceive in the future, while others damage or remove it.
Myomectomy is a surgery that allows your doctor to remove fibroids. There are numerous types of myomectomy. The optimal technique for you will be determined by the location, size, and number of fibroids you have. Myomectomy treatments to eliminate fibroids can include the following:
If you are not intending any further pregnancies, your healthcare professional may propose other options. These methods can be extremely helpful, but they usually prevent subsequent pregnancies. These may include:
Every treatment has some risks. Medicines can have side effects, and you might not be able to handle all of them. Before you start a new medication, you should tell your doctor about all the medicines you are already taking for other health problems and your full medical background. If you start taking a new drug and start to feel bad, call your doctor to talk about your choices.
Having surgery to remove fibroids also comes with some risks. You can get an infection or bleed during surgery, and there are also risks with anaesthesia. Another risk of surgery to remove a tumour is the chance of getting pregnant again. Some surgeries can stop women from getting pregnant again. A myomectomy only gets rid of the fibroids, so you can get pregnant again in the future. But people who have had a myomectomy might need a C-section to have another baby.
Most of the time, you can't avoid getting fibroids. One way to lower your chance is to keep a healthy weight and get regular pelvic exams. Make a plan with your doctor to check on your small tumours if you have them.
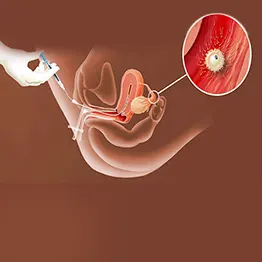
Uterine fibroids are benign (i.e. non-cancerous) growths arising from the muscle of the uterus. Small fibroids of 1-2 cms generally do not cause any symptoms. A fibroid can cause infertility when it is very large i.e. > 5 cms in diameter, it protrudes in the endometrial canal, or it causes a mechanical obstruction of the fallopian tube or the cervical canal. There are no medicines to cause a permanent cure of fibroid. However, GnRH analogues either in the form of daily or monthly injections for 4-6 months or nasal spray are used in the treatment of fibroids. This treatment can be useful to decrease the size of the fibroids before they can be operated upon. The treatment decreases the size of fibroid by 30-60%. Majority of the cases of fibroid need surgical treatment either laparoscopically or by the traditional cut on the abdomen. Fibroids situated in the cavity of the uterus are best operated upon through the Hysteroscopy.
Depending on the skill of the laparoscopic surgeon, Fibroids of all sizes can be operated laparoscopically. A cut is made on the bulge on the uterus where the fibroid is located. The fibroid is separated or dissected out. The defect on the uterus is sutured or closed laparoscopically. The fibroid is then taken out of the abdomen by cutting it into strips with the help of a morcellator. We have operated on fibroids of 12-15 cms at our setup. The pregnancy rates either natural or with treatment improves after a fibroid surgery.
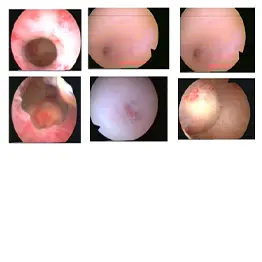
Hysteroscopy is useful to operate on fibroids that protrude into the cavity of uterus. The fibroid is cut into small strips with the help of energy source passed through resectoscope. The energy source could be either a bipolar or monopolar current. Bipolar current is safer. At our centre, we use a bipolar resectoscope for Hysteroscopic resection of the submucous fibroid.
We at Dr Sudha Tandon’s fertility, IVF, Gynec Endoscopy and Maternity center have all world class facilities for laparoscopic and hysteroscopic surgery for all pelvic pathologies and IUI /IVF and ICSI treatment for ART.
We are happy to have treated more than 20,000 couples with fertility issues. IUI is simple treatment for couples with unexplained Infertility, PCOS, early endometriosis Know More
Indicated in couples with tubal blockage, repeated failed IUI and endometriosis. Results range across 40 -50% at our centre Know More
Treatment of choice for male infertility with very low sperm count, obstructive azoospermia and for coupes requiring donor eggs. Know More
Many young men and women have utilized our fertility preservation services in the form of sperm, egg and embryo freezing either for medical or social reasons Know More

More than 3000 women have delivered at our centre. They have had an exceptional experience in antenatal care, delivery and postnatal care. Know More
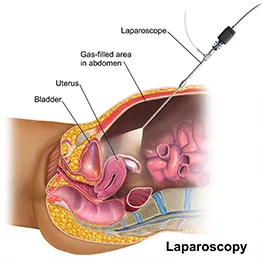
We have been performing all Gynaec surgeries through Laparoscopy for the past 25 years. Advantages are it is safe, less painful Know More
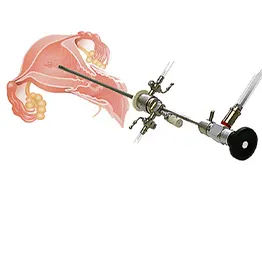
Hysteroscopy has many advantages over traditional D & C. We are equipped with small telescope to diagnose and treat pathologies inside the uterine cavity Know More
Fibroid causes infertility, pain and excessive menstrual blood loss. They can be operated through Laparoscopy or Hysteroscopy Know More
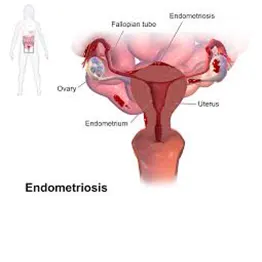
Endometriosis causes infertility and painful periods. Best treatment is initiated by Laparoscopy surgery and drugs Know More

We have been performing laparoscopic hysterectomy for the past 25 years. It is a definitive treatment for heavy menstrual bleeding, fibroids, cancer Know More
Ectopic is a condition where the pregnancy gets implanted in the fallopian tube instead of the uterine cavity. We have operated many cases laparoscopically Know More
Hysteroscopy helps in evaluating the cause of Postmenopausal bleeding Know More

MD. DGO.,
Gynaec Endoscopy Surgeon Fertility and IVF Consultant

M.S. Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound

MS, DNB Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound
-Very satisfied.
-Doc Support indeed was very good .
-Nurse Support was absolutely Beneficial and excellent.
-Cleanliness was upto the mark.
-Hospitality made the stay comfortable.
KEEP IT UP!
Harshita Chhajed
We were so ecstatic on 9thapril 2022 as we hold our baby boy in our hands. We are so grateful as we were in the bestest and safest hands. All this was possible because of the talented doctors like you all-Dr Sudha Tandon, Dr Aditi Tandon, Dr Amrita Tandon and Dr Sachin. Dr Sudha Tandon and DrAditi Tandon helped us in our pregnancy journey by making themselves available all the time on phone. All our queries/questions were answered in no time which is by far the best response we could have received during covid times.
All doctors have given us bestest suggestions during our pregnancy journey in which we always had an utmost faith. It was a great time spent with you all during this pregnancy.
Thankyou so much for all the help/assistance/suggestions. We will always recommend Dr Tandon to our friends and relatives.
Sheela C Potdar
Dr Sudha Tandon and her two daughters make you feel comfortable and at ease. The flow of the process was smooth without making the patients wait unnecessarily.
Ashrita Katyal
Staff very polite and cordial.
Clean and neat hospital.
Cheerful ambience.
Doctor was very cooperative understanding and most importantaly non-judgemental. Made talking easier.
Thankyou for this wonderful offer and for making these tests accessible to all.
Odette Fred
-Staff very pleasant and polite.
-Dr too very polite.
-No waste of time.
-Clean place.
-Gives a good feel and not a nervous hospital feel.
Rosa Fred
Dr Sudha Tandon is one of the most oldest and the bestgynac in Chembur. Very good initative taken by them to keep a watch on the womenshealth on the occasion of the womensday.glad to see her daughters doing the job same as their mom.
All the best to both of them.
Thankyou
Satpal Bhambri
Thankyou for arranging this camp and providing services at affordable prices. The entire doctors team and also everyone right from the front desk staff to the staff nurses are really very cordial and soft-spoken.
My mother literally has a OBGY phobia :-o yet when she stepped out of the consulting room,she only told me they are all really great especially Dr AditiMaam.
Keep up the good work! I always recommend your name whenever any relatives/friends ask for a good OBGY in town.
Thankyou
Regards,
Dr Aditi Prabhu
Pratima Prabhu
-Very well organized.
-The staff is very competent.
-Quick process without any difficulties.
-Excellent time Management.
Kavita Bhatti
It is always reassuring to talk to Dr Sudha Tandon, Dr Amrita and Dr Aditi. It is for their expert advise and their compassionate approach that makes me come back to them for all my health related concives. I know I am in good hands.
Sheetal Patil
Thank you for this camp. Was done professionally and good staff.
Thanks again.
Kavita R.
Got to hear from a friend about this women’s day camp. Very well organized camp by Dr Sudha Tandon.
The price works well for all.
Thank-you
Mrs. Harvinder Saggi
I was absolutely satisfied with Doctor Amrita’s Consultation.
She cleared all my queries.
Thank you for having this women’s day camp.
Its really helpful.
Gunwant Saggi
My mother has also been Dr Sudha Aunty’s patient and it was but natural for me to follow same.I would like too extend my gratitude and thanks to Dr Sudha aunty for being there for me at every step.My sincere thanks to Dr Aditi and Dr Amrita who have always had my back and responded to every query and doubt with great promptness. Dr Aditi has been my “go-to-person” in times of anxiety.
A big thank you to all three of there for everything. I couldn’t have pulled this off without your support.
Dr Jayeeta Verma
PCOS is a hormonal and Metabolic condition that affects women […]
04 Jun 22

IUI is a simple form of fertility treatment where motile […]
06 Aug 22
What is infertility ?
If the couple has regular intercourse, does not use any contraception and still does not conceive within one year, they are said to be infertile. 80-85% of the couples conceive within one year of unprotected intercourse i.e. without the use of any contraceptive. However, the rest 15-20 % who are unable to conceive naturally are said to be infertile and these would require proper evaluation and help for getting pregnant.
Does fertility depend on age?
Yes, in a woman fertility does depend on her age. A young woman is naturally more fertile as she has more number of good quality eggs than a woman who is 35 +. Hence a woman who is 35 + should not wait for a long period for a natural conception and should seek help from a proper fertility expert. Also the chance of genetic abnormalities and medical complications like Hypertension and Diabetes increases with age.
When should a couple seek medical help for infertility?
If the woman is below 35 years and has normal menstrual periods, and the couple has tried for a conception for a year with a frequency of sexual intercourse 3-4 times a week during the fertile period and has yet not conceive, then they need to consult an Infertility expert.
How does body weight, diet & exercise affect fertility?
For increasing the chance of pregnancy, balanced body weight of the woman would be beneficial. Being obese or grossly underweight affects the maturation of eggs in the woman and hence may affect her fertility. Also, a grossly obese woman would have mechanical difficulty in having normal sexual relations. Regular, moderate exercise especially in the form of yogasanas, walking, swimming, or jogging prove beneficial for fertility. It has been observed that strenuous form of exercises for example jogging over 3 miles a day can hamper ovulation and hence may lead to decrease in fertility in the woman. Balanced and nutritious diet help increase the chances of conception and ensure proper growth of the fetus.
Is stress a major factor in infertility?
Chronic stress may interfere with the ovulation, may decrease the sexual desire and hence affect the frequency of sexual intercourse in the couple.
How would one know the cause of infertility?
A detailed history of both partners is very helpful in giving a clue to the cause of infertility. For e.g. anovulation is the cause of infertility in a woman who has irregular periods and who is also obese, blocked fallopian tubes in a woman with previous history of pelvic infection, low sperm count in a man with past history of mumps. Examination of both the partners, and getting the required investigations would give a complete picture.
What are the most stressful stages of IVF?
A natural conception is obviously what all couples desire and wish when they plan a pregnancy but when it does not happen and the couple is counselled for an IVF treatment, it creates lots of stress for them.
The most stressful part is the acceptance of the fact that IVF is the only best option for their problem. A good discussion with the doctor to understand about Human Reproduction and why IVF is the best option for them to conceive will help the couple .They should take their time to understand about what the treatment involves and always ask questions to get their doubts cleared. A session with the counsellor would definitely help. Speaking to friends and family who are knowledgeable is a good way to reduce the stress but at times it could be counterproductive especially if they only talk of the problems and are themselves not positive.
In an IVF treatment, the woman’s eggs and her partner‘s sperms are fertilised in a laboratory. To get her eggs, she needs to take hormonal Injections on a daily basis and at the same time every day. This could create some stress especially if she is in a demanding job. It is best that she confides in someone who is reliable and understands the intricacies of an IVF treatment. The best part is that these Injections are not painful as very fine needles are used and she could also self-administer it.
She needs to see her fertility specialist for the follicular tracking for about 4-5 times in a cycle. This could also be demanding and stressful. She should just take all this in her stride and not get unduly stressed. The follicular response may not be satisfactory especially in a woman with poor ovarian reserve and she could become stressed.
She could have stress on the day of egg retrieval because of the fear of pain but this is a small procedure which is done under safe anaesthesia. The procedure is done through the vagina and there are no cuts on her abdomen. This is simple and safe procedure, not painful. At times the male partner gets stressed and is unable to give his semen sample on the day of egg pickup. To avoid this problem, almost all fertility centres will freeze the semen sample beforehand as a backup.
Of course the other stressful point is to worry about the numbers and quality of eggs got at the time of pickup, the fertilization of the eggs, and the numbers of good quality embryos. All these are important form success point of view. A communication with the couple before the procedure will allay all their fears and will go a long way in taking care of the stress.
The most important step in IVF Treatment
The most important step in IVF is Embryo transfer for which the woman should relax. Generally it is done without anaesthesia. The woman‘s cooperation is so very important for favourable results.
After the embryo transfer one has to wait for about 10 days to know the results. It could be very stressful at this stage. She should try to be calm and not just keep thinking of the results. After the embryo transfer the woman has to use either progesterone vaginal tablets or Injections and the stress of finances adds to the stress of procedure.
All in all we do understand the stress that the couple undergoes for an IVF treatment cycle. Have trust in your doctor and you would definitely become a successful.
At our IVF Clinic in Mumbai and IVF centre in Navi Mumbai, we spend quite a lot of time to make you feel comfortable. Our entire support staff and our embryologist are in constant touch with the couple. We try to see that you do not have to wait for too long to see the doctor. We have all facilities of Hysteroscopy/ Laparoscopy / IVF treatment and Maternity at Dr Sudha Tandon centre and we take utmost care of our patients.