Hysteroscopy in Infertility
Hysteroscopy is the examination of the uterine cavity with a telescope using a continuous flow of fluid for distension. With the advent of smaller diameter Hysteroscopes, it has become possible to diagnose and treat a variety of uterine pathologies using an office hysteroscope. Office Hysteroscopy as the name suggests is a procedure which can be done on an outpatient basis. This offers accurate diagnosis with minimal pain and discomfort to the patient.
ADVANTAGES
- The smaller diameter of the hysteroscope and instruments causes less pain while maintaining efficacy for visualization.
- Immediate return to routine activities.
- The vaginoscopic approach is followed, hence there is no need to hold the cervix and does not require cervical dilatation.
TECHNIQUE
The instruments required for office hysteroscopy include the hysteroscope with an outer diameter of 4 to 5.5mm, camera, light source, continuous inflow, and outflow, along with graspers, scissors, biopsy forceps, and bipolar cautery. Normal saline is used as distension media using pressure bags for infusion.
Bettocchi and Selvaggi introduced the vaginoscopic method where the hysteroscope is first placed in the posterior fornix, distending the vagina. Then it is slightly withdrawn to reach the cervical opening. The scope is then introduced into the cervical canal under vision. Paracervical block is not necessary.

USES
1.Diagnostic hysteroscopy – in patients of unexplained infertility, or an ultrasound/HSG suggestive of uterine pathology, visualizing the uterine cavity prior to IUI / IVF cycles is imperative. This not only helps asses the condition of the uterine cavity, but several procedures which are later discussed can be performed.

2. Hysteroscopic Polypectomy- endometrial polyps which can hinder normal implantation, can be removed.
3. Metroplasty – Uterine septum is a cause of repeated implantation failure and repeated first trimester abortions. A small uterine septum can be cut using scissors during office hysteroscopy. T shaped uterus and narrow cavities can be corrected by doing lateral metroplasty. This increases the size of the cavity and may help improve pregnancy rates.

4. Adhesiolysis – Asherman’s syndrome is seen patients who have had tuberculosis, or multiple D and Cs. This leads to intrauterine adhesions and implantation failures. Correcting this is possible using scissors.
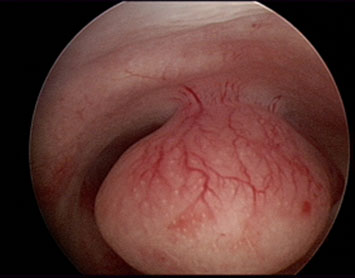
5. Submucous fibroids – they are a cause of infertility and poor pregnancy outcomes. Treating fibroids surgically has proven to improve live pregnancy rates. Hysteroscopic myomectomy can be done using monopolar/bipolar current or with scissors after applying traction.

6. Tubal cannulation – unilateral or bilateral proximal tubal occlusion is documented in 10 to 20% of Hysterosalpingography (HSG) performed during an initial infertility workup. This can be corrected by cannulation during hysteroscopy.
We at Dr. Sudha Tandon Fertility, IVF, Endoscopy and Maternity Centre, have all the facilities and experienced doctors for hysteroscopy. We routinely do hysteroscopies for many infertile patients, especially those requiring IVF, with repeated implantation failures. It is a short procedure and patients are discharged the same day within a few hours postoperatively.