
Dr. Sudha Tandon
Gynaec Endoscopic Surgeon and IVF Consultant
M.D.,D.G.O
Director, Dr. Sudha Tandon Fertility, IVF, Endoscopy & Maternity Centre.

Dr. Amrita Tandon
MS, DNB, FMAS, MRM Reproductive Medicine (London)
Gynaec Endoscopic Surgeon and IVF Consultant ,
Dr. Sudha Tandon Fertility, IVF, Endoscopy & Maternity Centre.
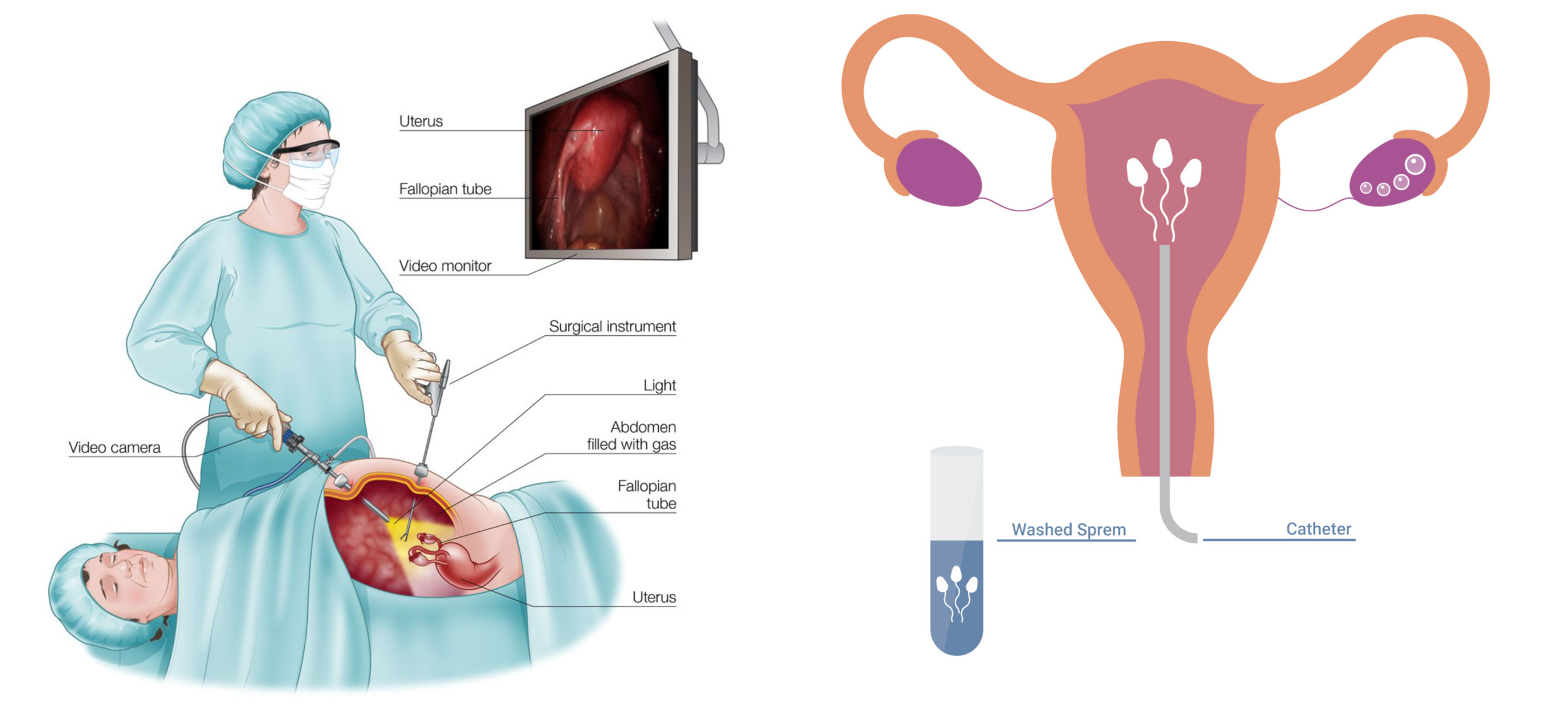
Hysteroscopy and Laparoscopy both have a definitive role in the management of infertility and ART . Intrauterine insemination ( IUI ) warrants the presence of a fairly normal reproductive pelvic organ structure and function , especially the patency of the fallopian tubes. The role of endoscopic surgery has been established before IUI in case of known correctable pelvic pathology. It’s role has been debated in case of unexplained infertility especially when there is failure of IUI due to unknown reasons .
Advances in imaging techniques with 2 dimensional and 3 dimensional ultrasound, saline infusion sonography, computerized tomography (CT), and magnetic resonance imaging (MRI) for the evaluation of uterine and pelvic disease have decreased the use of diagnostic hystero-laparoscopy as a first line investigation in patients with infertility. Hysterosalpingography (HSG) and hysterosalpingo-contrast-sonography (HyCoSy) are inexpensive, lesser invasive, well-tolerated methods of determining tubal patency, but their accuracy compared to laparoscopy is a matter of debate. A number of studies suggest that diagnostic hystero-laparoscopy may be of additional value over the standard first line investigations, because it indicates intra-abdominal pathologic abnormalities in 36 - 68 % of cases even after a normal HSG. It is accepted as the most accurate method for evaluating tubal pathological and other pelvic causes of infertility. 1
A study published in Fertility and Sterility (2003) to evaluate the accuracy of diagnostic laparoscopy after normal hysterosalpingography (HSG) and before intrauterine insemination (IUI) with respect to laparoscopic findings leading to a change of treatment decisions in couples with male subfertility, cervical factor, or unexplained infertility concluded that in about 25% of the couples, it led to an alteration in treatment plan. In 21%, intervention was done at the time of diagnostic laparoscopy in terms of adhesiolysis of periadnexal adhesions and treatment of minimal and mild endometriosis with consequent IUI. This also eventually led to an overall increase in live birth rates. Most studies have shown the benefit of laparoscopic surgery for minimal and mild endometriosis prior to IUI. 2
An Indian study by Jayakrishnan et al 3 in 2010, evaluated the role of Hysterolaparoscopy in patients who had no detectable pathology based on history, physical examination, and ultrasound and had treatment for three or more cycles in the form of ovulation induction and IUI. They reviewed 127 patients who fulfilled the inclusion criteria. Of the 127 women, 12.6% (n= 16) had no detectable pathology on laparohysteroscopy. The incidence of endometriosis was 77.2% (n= 98); of which 70.9 % had minimal to mild disease. No cases with Stage IV disease were present. 5.5% of patients had pelvic inflammatory disease (PID) with unilateral and bilateral tubal adhesions and tubal blocks. There were no abnormal findings at hysteroscopy.
Endoscopic surgery is invasive and requires the use of general anaesthesia and hence is not without risk of complications. In the recent era of Assisted Reproductive Technologies (ART), the easy availability and faster results of In Vitro Fertilisation (IVF) have led to the decline in use of laparoscopy due to the added expense and possible complications. But it is important to note that the cost of IVF is high and one attempt usually offers only one chance of successful pregnancy . On the contrary in a young infertile woman < 35 years of age, with treatable pelvic pathology, laparoscopic correction can help improve the chance of natural conception and success rates of IUI.
The timing of endoscopic surgery in the management of infertility has been a matter of debate. Performing a laparoscopy prior to initiating treatment looks attractive, but the cost of this surgical procedure is high. Mostfertility specialists thus prefer to treat couples with unexplained infertility with a few cycles of ovulation stimulation with IUI before proceeding to laparoscopy.
A prospective randomized reallocation study to investigate the timing of laparoscopy after a normal hysterosalpingography was performed 4. This study, however, showed no significant difference in the prevalence of abnormalities with clinical consequences at laparoscopy before IUI when compared to laparoscopy after six cycles of IUI. It concluded that the impact of the detection and the laparoscopic treatment of observed pelvic pathology prior to IUI did not seem to affect IUI outcome. The authors raised doubts about the value of routinely performing a diagnostic and/or therapeutic laparoscopy prior to IUI treatment.
1.ENDOMETRIOSIS SURGERY : The most common finding on laparoscopy in patients who are unable to conceive with IUI and apparently normal findings on imaging techniques is minimal to mild endometriosis. The possible reasons for subfertility in endometriosis include dyspareunia and alterations in pelvic anatomy and peritoneal and tubal environments. Other proposed mechanisms include interference with fertilisation, oocyte and embryo development, and implantation.
More severe forms of endometriosis which include endometriosis and deeply infiltrating endometriosis are diagnosed accurately with clinical examination and ultrasound and or MRI. Laparoscopy is the gold standard for more subtle lesions of endometriosis like superficial endometriosis. These superficial lesions can be treated with ablation (electrocautery or laser) or excision and adhesiolysis to restore the tuba-ovarian anatomy during laparoscopy. For endometriomas, the management has been controversial. Most International guidelines suggest endometriotic cyst excision over drainage of a cyst above the size of 4cm prior to IVF, but there is risk of reduction in ovarian reserve. Most ART specialists prefer IVF over surgical treatment of endometriomas. There is limited evidence on the treatment of endometriomas prior to IUIand most clinicians would recommend surgery followed by natural conception or IVF in women with endometriomas 5
Surgery for Deep infiltrating endometriosis is recommended only for symptom relief and has not shown to improve pregnancy rates with or without ART.
Proximal tubal blockage accounts for 10%–25% of tubal disease . It may be due to obstruction resulting from plugs of mucus and amorphous debris, due to spasm of the uterotubal ostium, or due to occlusion, which is a true anatomic blockage from fibrosis due to salpingitis isthmica nodosa (SIN), pelvic inflammatory disease , or endometriosis. Tubal cannulation to treat proximal tubal block can be done via hysteroscopy with laparoscopic confirmation . This should be attempted only if distal tubal pathology is ruled out. Gentle pressure is needed the to overcome the obstruction by tubal cannulation, and if force is required then a true anatomic occlusion is assumed and the procedure should be aborted 6.
A meta-analysis of studies treating patients with bilateral proximal tubal occlusion showed that the obstruction is relieved in approximately 85% of the tubes with tubal cannulation and that approximately half of the patients conceive 7.
Surgery for Distal Tubal disease : Distal tubal disease includes hydrosalpinx and fimbrial phimsosis. A good prognosis is seen with patients who have no more than limited filmy adnexal adhesions, mildly dilated tubes (<3 cm) with thin and pliable walls, and a lush endosalpinx with preservation of the mucosal folds. Laparoscopic neosalpingostomy and fimbrioplasty are carried out by opening a hydrosalpinx or increasing the opening for fimbrial phimosis, respectively. Pregnancy rates after these procedures depend on the degree of tubal disease and are more favorable with good-prognosis patients. Intrauterine and ectopic pregnancy rates after neosalpingostomy for mild hydrosalpinges range from 58% to 77% and from 2% to 8%, respectively 8. There is no evidence to state that IUI treatment increases the pregnancy rates over expectancy management after tubal surgery.
Tubal surgery is the first-line management option for young women less than 35-years-old with minor tubal pathology. The second option should be IVF if there are other factors affecting fertility, if the patient is >38-years-old, if patient had moderate to severe tubal disease, and if one year or more had passed post-surgery for tubal pathology.9
Laparoscopic Ovarian Drilling (LOD):
The proposed mechanisms by which LOD helps is by destruction of androgen producing stroma, causing reduction in the intraovarian and circulating levels of androgens and LH.
PCOS women who have a high LH value , lean PCOS and non-insulin resistant are known to have a better response to LOD. It is usually done in women who are resistant to clomiphene citrate as an alternative to use of gonadotropins. Use of gonadotropins with IUI is second line treatment in CC - resistant PCOS women. As per Cochrane review 2012, it was found that LOD is as effective as ovulation induction in terms of clinical pregnancy or live birth rates, but risk of multiple pregnancy is lower with LOD 10 . The concerns about LOD are risk of adhesions and ovarian failure following LOD. The hilar region should be avoided and the ovary should be raised before the application of energy and saline wash should be done after the procedure to lower the risk of injury. The usual dictum is application of 4 diathermy points to each ovary for 4 seconds each , and using a power of 40W. 11
Regarding the efficacy of ovarian drilling, observational studies demonstrated that the ovulation rate was between 54 and 76% in the 6 months after the procedure and 33 and 88% in the 12 months after the procedure. During these periods, the spontaneous pregnancy rate ranged between 28 and 56% and 54 and 70%, respectively. 12
REPRODUCTIVE
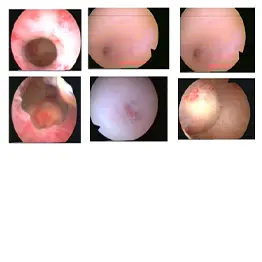
HYSTEROSCOPIC SURGERY PRIOR TO IUI:
Hysteroscopy is the most accurate method to diagnose and treat unsuspected and subtle intrauterine pathologies in the infertile women. Uterine pathologies like endometrial polyps, uterine septa, intrauterine adhesions and submucosal fibroids cause infertility by impairing embryo implantation and growth due to poor vascularisation , affecting sperm migration, or by causing an inflammatory endometrial response.
Hysteroscopic Polypectomy :
Perez-Medina et al.13 randomised women with a clear sonographic diagnosis of endometrial polyps and at least 1 year of infertility to hysteroscopy and polypectomy or diagnostic hysteroscopy and polyp biopsy prior to planned intrauterine insemination (IUI) treatment. The mean polyp diameter in the treated group was 16 mm (3–24 mm). The pregnancy rates after four cycles of stimulated IUI starting at least 3 months after surgery were significantly higher in the polypectomy group (63% versus 28%).
Similarly in another study by Kalampokas et al 14 study group consisted of 86 women who, following the diagnosis of endometrial polyp, underwent hysteroscopic polypectomy and the control group consisted of 85 women who chose not to undergo polypectomy before IUI. There was a statistically significant difference in cumulative pregnancy rates between the two groups. The group that underwent polyp removal had higher pregnancy rates as compared to the one that the polyps were left intact following IUI. Hence , hysteroscopic removal of polyps has shown to improve the pregnancy rates after IUI .
Intrauterine adhesions :
A more recent study by Chen et al 15 evaluated the reproductive outcomes in 357 patients with mild, moderate, and severe Asherman’s syndrome who underwent hysteroscopic adhesiolysis. The reproductive outcomes of 332 women (93%) were followed for an average duration of 27±9 months, and the overall conception rate after hysteroscopic adhesiolysis was 48.2%, which decreased with increased intrauterine adhesions (IUA) severity (mild, 60.7%; moderate, 53.4%; severe, 25%). The mean time to conception following hysteroscopic adhesiolysis was 9.7±3.7 months. The miscarriage rate was 9.4%, and the live birth rate was no lower than 85.6%. Eleven patients (7.9%) had postpartum hemorrhage, including 6 (4.3%) due to adherent placenta and 3 (2.1%) due to placenta accreta.Hysteroscopic adhesiolysis is a feasible and effective way to improve fertility in patients with Asherman's syndrome.
Hysteroscopic division of adhesions with scissors or electrosurgery is usually recommended. Some women may require multiple procedures to achieve a satisfactory anatomical result due to the high recurrence rate. Second Look hysteroscopy with re-adhesiolysis is usually recommended. Postoperative mechanical distension of the uterine cavity with an intrauterine device or a paediatric foley’s catheter along with oestrogen therapy to facilitate endometrial regrowth and proliferation are commonly used to decrease the high rate of recurrence.
OTHER ENDOSCOPIC SURGERIES:
The other fertility enhancing endoscopic surgeries like hysteroscopic myomectomy for submucosal fibroids, hysteroscopic septal resection, laparoscopic myomectomy are known to improve fertility outcomes and hence indirectly also improve success rates of IUI.
To conclude, endoscopic surgeries have a role in optimising the outcome of IUI , provided, done for the correct indication, and with standard techniques as suggested by research.
Couples who fail to conceive with ovulation stimulation with IUI should be counselled that there is evidence to show that laparoscopy is of benefit before proceeding to IVF . At the same time, the use of empirical treatment in the form of ovulation stimulation and IUI prior to laparoscopy might reduce the number of patients requiring the procedure, reduce the number of negative laparoscopies, and optimize resource utilization.
REFERENCES:
PCOS is a hormonal and Metabolic condition that affects women […]
04 Jun 22

IUI is a simple form of fertility treatment where motile […]
06 Aug 22
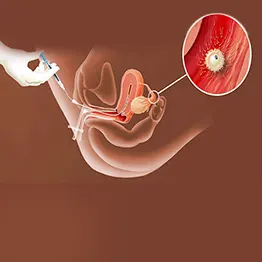
We are happy to have treated more than 20,000 couples with fertility issues. IUI is simple treatment for couples with unexplained Infertility, PCOS, early endometriosis Know More
Indicated in couples with tubal blockage, repeated failed IUI and endometriosis. Results range across 40 -50% at our centre Know More
Treatment of choice for male infertility with very low sperm count, obstructive azoospermia and for coupes requiring donor eggs. Know More
Many young men and women have utilized our fertility preservation services in the form of sperm, egg and embryo freezing either for medical or social reasons Know More

More than 3000 women have delivered at our centre. They have had an exceptional experience in antenatal care, delivery and postnatal care. Know More
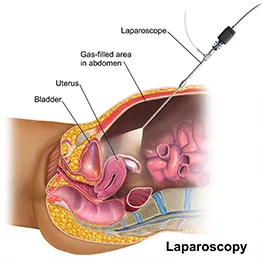
We have been performing all Gynaec surgeries through Laparoscopy for the past 25 years. Advantages are it is safe, less painful Know More
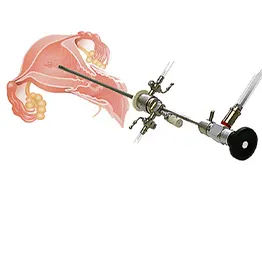
Hysteroscopy has many advantages over traditional D & C. We are equipped with small telescope to diagnose and treat pathologies inside the uterine cavity Know More
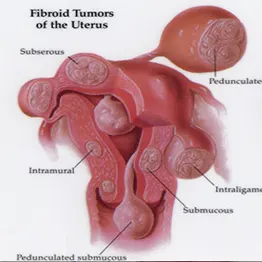
Fibroid causes infertility, pain and excessive menstrual blood loss. They can be operated through Laparoscopy or Hysteroscopy Know More
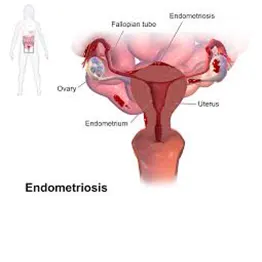
Endometriosis causes infertility and painful periods. Best treatment is initiated by Laparoscopy surgery and drugs Know More

We have been performing laparoscopic hysterectomy for the past 25 years. It is a definitive treatment for heavy menstrual bleeding, fibroids, cancer Know More
Ectopic is a condition where the pregnancy gets implanted in the fallopian tube instead of the uterine cavity. We have operated many cases laparoscopically Know More
Hysteroscopy helps in evaluating the cause of Postmenopausal bleeding Know More

MD. DGO.,
Gynaec Endoscopy Surgeon Fertility and IVF Consultant

M.S. Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound

MS, DNB Obgy,
Fellowship in Reproductive Medicine and IVF (London), Minimal Access Surgery and Ultrasound
-Very satisfied.
-Doc Support indeed was very good .
-Nurse Support was absolutely Beneficial and excellent.
-Cleanliness was upto the mark.
-Hospitality made the stay comfortable.
KEEP IT UP!
Harshita Chhajed
We were so ecstatic on 9thapril 2022 as we hold our baby boy in our hands. We are so grateful as we were in the bestest and safest hands. All this was possible because of the talented doctors like you all-Dr Sudha Tandon, Dr Aditi Tandon, Dr Amrita Tandon and Dr Sachin. Dr Sudha Tandon and DrAditi Tandon helped us in our pregnancy journey by making themselves available all the time on phone. All our queries/questions were answered in no time which is by far the best response we could have received during covid times.
All doctors have given us bestest suggestions during our pregnancy journey in which we always had an utmost faith. It was a great time spent with you all during this pregnancy.
Thankyou so much for all the help/assistance/suggestions. We will always recommend Dr Tandon to our friends and relatives.
Sheela C Potdar
Dr Sudha Tandon and her two daughters make you feel comfortable and at ease. The flow of the process was smooth without making the patients wait unnecessarily.
Ashrita Katyal
Staff very polite and cordial.
Clean and neat hospital.
Cheerful ambience.
Doctor was very cooperative understanding and most importantaly non-judgemental. Made talking easier.
Thankyou for this wonderful offer and for making these tests accessible to all.
Odette Fred
-Staff very pleasant and polite.
-Dr too very polite.
-No waste of time.
-Clean place.
-Gives a good feel and not a nervous hospital feel.
Rosa Fred
Dr Sudha Tandon is one of the most oldest and the bestgynac in Chembur. Very good initative taken by them to keep a watch on the womenshealth on the occasion of the womensday.glad to see her daughters doing the job same as their mom.
All the best to both of them.
Thankyou
Satpal Bhambri
Thankyou for arranging this camp and providing services at affordable prices. The entire doctors team and also everyone right from the front desk staff to the staff nurses are really very cordial and soft-spoken.
My mother literally has a OBGY phobia :-o yet when she stepped out of the consulting room,she only told me they are all really great especially Dr AditiMaam.
Keep up the good work! I always recommend your name whenever any relatives/friends ask for a good OBGY in town.
Thankyou
Regards,
Dr Aditi Prabhu
Pratima Prabhu
-Very well organized.
-The staff is very competent.
-Quick process without any difficulties.
-Excellent time Management.
Kavita Bhatti
It is always reassuring to talk to Dr Sudha Tandon, Dr Amrita and Dr Aditi. It is for their expert advise and their compassionate approach that makes me come back to them for all my health related concives. I know I am in good hands.
Sheetal Patil
Thank you for this camp. Was done professionally and good staff.
Thanks again.
Kavita R.
Got to hear from a friend about this women’s day camp. Very well organized camp by Dr Sudha Tandon.
The price works well for all.
Thank-you
Mrs. Harvinder Saggi
I was absolutely satisfied with Doctor Amrita’s Consultation.
She cleared all my queries.
Thank you for having this women’s day camp.
Its really helpful.
Gunwant Saggi
My mother has also been Dr Sudha Aunty’s patient and it was but natural for me to follow same.I would like too extend my gratitude and thanks to Dr Sudha aunty for being there for me at every step.My sincere thanks to Dr Aditi and Dr Amrita who have always had my back and responded to every query and doubt with great promptness. Dr Aditi has been my “go-to-person” in times of anxiety.
A big thank you to all three of there for everything. I couldn’t have pulled this off without your support.
Dr Jayeeta Verma
What is infertility ?
If the couple has regular intercourse, does not use any contraception and still does not conceive within one year, they are said to be infertile. 80-85% of the couples conceive within one year of unprotected intercourse i.e. without the use of any contraceptive. However, the rest 15-20 % who are unable to conceive naturally are said to be infertile and these would require proper evaluation and help for getting pregnant.
Does fertility depend on age?
Yes, in a woman fertility does depend on her age. A young woman is naturally more fertile as she has more number of good quality eggs than a woman who is 35 +. Hence a woman who is 35 + should not wait for a long period for a natural conception and should seek help from a proper fertility expert. Also the chance of genetic abnormalities and medical complications like Hypertension and Diabetes increases with age.
When should a couple seek medical help for infertility?
If the woman is below 35 years and has normal menstrual periods, and the couple has tried for a conception for a year with a frequency of sexual intercourse 3-4 times a week during the fertile period and has yet not conceive, then they need to consult an Infertility expert.
How does body weight, diet & exercise affect fertility?
For increasing the chance of pregnancy, balanced body weight of the woman would be beneficial. Being obese or grossly underweight affects the maturation of eggs in the woman and hence may affect her fertility. Also, a grossly obese woman would have mechanical difficulty in having normal sexual relations. Regular, moderate exercise especially in the form of yogasanas, walking, swimming, or jogging prove beneficial for fertility. It has been observed that strenuous form of exercises for example jogging over 3 miles a day can hamper ovulation and hence may lead to decrease in fertility in the woman. Balanced and nutritious diet help increase the chances of conception and ensure proper growth of the fetus.
Is stress a major factor in infertility?
Chronic stress may interfere with the ovulation, may decrease the sexual desire and hence affect the frequency of sexual intercourse in the couple.
How would one know the cause of infertility?
A detailed history of both partners is very helpful in giving a clue to the cause of infertility. For e.g. anovulation is the cause of infertility in a woman who has irregular periods and who is also obese, blocked fallopian tubes in a woman with previous history of pelvic infection, low sperm count in a man with past history of mumps. Examination of both the partners, and getting the required investigations would give a complete picture.
What are the most stressful stages of IVF?
A natural conception is obviously what all couples desire and wish when they plan a pregnancy but when it does not happen and the couple is counselled for an IVF treatment, it creates lots of stress for them.
The most stressful part is the acceptance of the fact that IVF is the only best option for their problem. A good discussion with the doctor to understand about Human Reproduction and why IVF is the best option for them to conceive will help the couple .They should take their time to understand about what the treatment involves and always ask questions to get their doubts cleared. A session with the counsellor would definitely help. Speaking to friends and family who are knowledgeable is a good way to reduce the stress but at times it could be counterproductive especially if they only talk of the problems and are themselves not positive.
In an IVF treatment, the woman’s eggs and her partner‘s sperms are fertilised in a laboratory. To get her eggs, she needs to take hormonal Injections on a daily basis and at the same time every day. This could create some stress especially if she is in a demanding job. It is best that she confides in someone who is reliable and understands the intricacies of an IVF treatment. The best part is that these Injections are not painful as very fine needles are used and she could also self-administer it.
She needs to see her fertility specialist for the follicular tracking for about 4-5 times in a cycle. This could also be demanding and stressful. She should just take all this in her stride and not get unduly stressed. The follicular response may not be satisfactory especially in a woman with poor ovarian reserve and she could become stressed.
She could have stress on the day of egg retrieval because of the fear of pain but this is a small procedure which is done under safe anaesthesia. The procedure is done through the vagina and there are no cuts on her abdomen. This is simple and safe procedure, not painful. At times the male partner gets stressed and is unable to give his semen sample on the day of egg pickup. To avoid this problem, almost all fertility centres will freeze the semen sample beforehand as a backup.
Of course the other stressful point is to worry about the numbers and quality of eggs got at the time of pickup, the fertilization of the eggs, and the numbers of good quality embryos. All these are important form success point of view. A communication with the couple before the procedure will allay all their fears and will go a long way in taking care of the stress.
The most important step in IVF Treatment
The most important step in IVF is Embryo transfer for which the woman should relax. Generally it is done without anaesthesia. The woman‘s cooperation is so very important for favourable results.
After the embryo transfer one has to wait for about 10 days to know the results. It could be very stressful at this stage. She should try to be calm and not just keep thinking of the results. After the embryo transfer the woman has to use either progesterone vaginal tablets or Injections and the stress of finances adds to the stress of procedure.
All in all we do understand the stress that the couple undergoes for an IVF treatment cycle. Have trust in your doctor and you would definitely become a successful.
At our IVF Clinic in Mumbai and IVF centre in Navi Mumbai, we spend quite a lot of time to make you feel comfortable. Our entire support staff and our embryologist are in constant touch with the couple. We try to see that you do not have to wait for too long to see the doctor. We have all facilities of Hysteroscopy/ Laparoscopy / IVF treatment and Maternity at Dr Sudha Tandon centre and we take utmost care of our patients.